Written and reviewed for scientific and factual accuracy by Dr. Austin Jelcick, PhD and Dr. Matthew Janzen, DC. Last reviewed/edited on March 10, 2020.
Mild scoliosis refers to an idiopathic scoliosis curve measuring less than 20 degrees. In the past, children and teens with mild scoliosis were often advised to “watch and wait,” taking periodic x-rays every 6–12 months to monitor progression. But research shows that this passive approach isn’t ideal. Mild scoliosis can worsen quickly, especially during growth spurts. So what should you do about mild scoliosis? Are there early symptoms or signs that a mild spinal curve could develop into moderate scoliosis or severe scoliosis? Understanding the risks and the probability of curve progression is key to choosing the right mild scoliosis treatment and preventing future complications.
The good news is that the best time to treat a scoliosis is when it is mild: when the curve is small and the child is young and skeletally immature
Research shows that early detection and early intervention when curves are small provides better treatment outcomes 1-3, so let’s learn why and also see what warning signs we can look out for so idiopathic scoliosis never sneaks up on us.
Mild scoliosis: How easy is it to detect?
Detecting a mild scoliosis can be a challenging task for several reasons. You might think that when a curve is present in the spine that a child or teen might have some pain but this isn’t the case. In fact, it is quite rare for kids to feel pain when they have scoliosis even when the curve is quite large 4. Because the scoliosis is idiopathic, there aren’t typically any other health problems.
In contrast, when scoliosis is neuro-muscular or congenital there are often other problems such as in neuro-muscular patients who often are unable to walk around on their own 5.
Because mild scoliosis often has no symptoms, many groups have worked to catch cases early through proactive school screenings. However even this has proven difficult due to problems with the screening process. Sadly, these problems and the inaccuracy of traditional school screenings have resulted in several states in the US ending their school screening programs.
Why Traditional Screening Falls Short
Any good screening method should have excellent sensitivity and excellent specificity. Sensitivity measures how well positive cases (kids who actually HAVE scoliosis) are detected, while specificity measures how well negative cases (kids who DON’T have scoliosis) are detected.
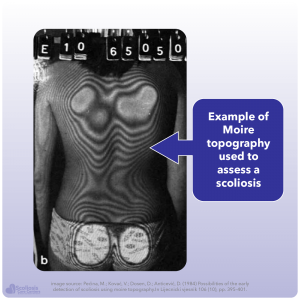
The “gold standard” for scoliosis screening across the world has traditionally been one or more of the four following tests 6:
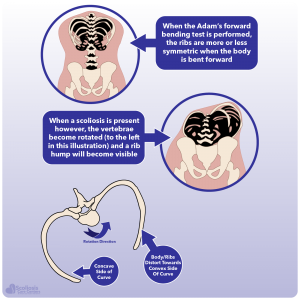
- Adam’s forward bending test
- Measuring rotation with a scoliometer
- Measuring any rib hump that is present
- Using moiré topography to make a 3D image of the back
You might wonder why we use all these different screening tests instead of simply taking an x-ray of the spine to see if a curve is present. The problem with taking x-rays for screening is the same reason why so many doctors traditionally used “watch and wait” even when kids were getting worse: radiation.
The problem of x-ray in screening
The concept of “watch and wait” and only checking the spine with x-ray every 6 to 12 months isn’t because we only need to look once or twice a year but rather it is an attempt to limit radiation from the x-ray. Studies have shown increased risks of cancer for those with scoliosis due to all of the x-rays they are exposed to over their lifetime 7. Thus, in an effort to limit radiation exposure, doctors only look every 6 to 12 months.
Doctors avoid using x-rays for scoliosis screenings to limit radiation exposure. This concern is also one reason some states have stopped school screenings (more on this later).
Challenges with Other Screening Methods
Because x-ray is essentially condemned due to the potential harm to the child (and the cost 6), screening for and detecting a mild scoliosis has to rely on other methods like the four we mentioned earlier. Unfortunately, these methods vary in their accuracy and frequently result in a high number of false positives.
While a false positive might not seem serious, it leads to unnecessary referrals. When a child screens positive, doctors take an x-ray to confirm the diagnosis. This exposes kids to harmful radiation when they might not need it. False negatives are also dangerous. In those cases, a child with scoliosis goes unnoticed, and their curve worsens without treatment.
Why School Screenings Have Declined
If screening for a mild scoliosis curve doesn’t allow x-ray and the standard methods of screening result in false. School screenings cost money, and many kids got x-rays even though they didn’t have scoliosis8. Thus, school districts and states found it easy to cut screening out of the budget such as with California which hasn’t had school scoliosis screenings since 2010.
What is the chance that a mild scoliosis becomes severe or requires surgery?
One of the biggest problems with scoliosis is that it can get rapidly worse when a child goes through their growth spurt during puberty: the adolescent growth spurt. The problem here is that if a child has a mild scoliosis when they are young, but it won’t get drastically worse until they hit their adolescent growth spurt, how can we know whether or not we should take action? If science shows treatment is more successful when curves are small and the child is young, how can we know we need to act now?
Thankfully, recent research has come up with mathematical equations that we can use to predict whether a curve will get worse (progress) and whether or not it will progress to the point that it needs surgery.
To summarize, researchers create these equations—often called prognostic models—by studying patients with untreated idiopathic scoliosis. They look for variables that influence whether curves worsen, and whether they progress into the surgical range (40–50 degrees). While not perfect, these models provide a strong, science based probability that a curve will worsen.
What is the chance that a small curve will progress?
The first question most people have before they worry about surgery is simply wondering whether or not their curve or their child’s curve will get worse. When a curve gets worse, we commonly refer to it as “progressing”. Thus determining the probability of curve progression is important because it lets us know how likely it is that the scoliosis curve will get worse.
When we look at the scientific model for curve progression, it is first important to define what we mean by progression: if the curve gets worse, how much worse will it get? The criteria that is used is based on the initial size of the curve. For curves 19 degrees or less, progression is defined as an increase of at least 10 degrees where the curve is bigger than 20 degrees at the end. Similarly for curves 20-29 degrees (or larger) progression is defined as an increase of at least 5 degrees or more 9.
We define progression as a curve increasing by 10° or more when starting at 19° or less, or by 5° or more when starting between 20° and 29°.
Using these criteria we can approximate the likelihood that a mild scoliosis curve will progress, keeping in mind that to be “mild” our curve needs to be less than 20 degrees to begin with. Also remember: doctors only diagnose scoliosis when a curve measures greater than 10 degrees. Last but not least while a child’s age can be important, their bone age (skeletal maturity) is even more important because it lets us know approximately how much growth they have left (scoliosis gets worse as a child hits their growth spurts). So what do our chances of progression look like?
| Age | Risser | Curve Size | Probability of Progression |
|---|---|---|---|
| 5 | 0 | 10 | 85% |
| 5 | 0 | 12 | 98% |
| 10 | 0 | 10 | 15% |
| 10 | 0 | 12 | 27% |
| 10 | 0 | 15 | 50% |
| 10 | 0 | 18 | 73% |
Risk of Progression in Mild Scoliosis
| Age | Risser | Curve Size | Probability of Progression |
|---|---|---|---|
| 12 | 2 | 10 | 0% |
| 12 | 2 | 14 | 3% |
| 12 | 2 | 18 | 15% |
| 14 | 2 | 10 | 0% |
| 14 | 2 | 14 | 1% |
| 14 | 2 | 18 | 9% |
What is the chance that a small curve will need surgery?
While calculating the probability that a curve will worsen is important, it doesn’t answer the question that is on every parents’ mind when they first learn their child has scoliosis: will the curve need surgery? To determine the chance that a mild scoliosis will worsen to the point that surgery is needed (40-50 degrees) we need a new equation 10.
While our progression calculator is based on the size of the curve, how old the child is, and how skeletally mature they are, to calculate the probability of surgery we need to know something else: the location of the curve. The likelihood that a curve will require surgery drastically increases when the curve is located in the thoracic area of the spine. If a curve is located in the lumbar or thoracolumbar region the chances of surgery decrease. It’s also interesting to know that we only need to know how skeletally mature the child is and not how old they actually are; this is simply because the child’s age wasn’t found to be significantly associated with the risk of surgery.
Let’s look at some examples and see how our risk of surgery changes depending on the size and location of the curve, as well as the skeletal age of the child. Keep in mind that Risser and Sander’s score/scale are simply two different methods of determining skeletal maturity: the lower the number, the less mature the child is. It is also useful to know that a young girl who is a 2 on the Sanders scale (2 out of 8) has JUST STARTED her adolescent growth spurt but has not yet reached her fastest rate of growth during puberty.
The Risser and Sander’s scale are two different ways to determine skeletal maturity
| Sanders Score | Curve Size | Curve Location | Probability of Surgery |
|---|---|---|---|
| 1-2 | 11 | Lumbar/thoracolumbar | 3.60% |
| 1-2 | 15 | Lumbar/thoracolumbar | 9.04% |
| 1-2 | 19 | Lumbar/thoracolumbar | 20.91% |
| 1-2 | 11 | Any thoracic curve | 13.26% |
| 1-2 | 15 | Any thoracic curve | 28.91% |
| 1-2 | 19 | Any thoracic curve | 51.96% |
Again, this is for young skeletally immature kids. This again makes sense because if the curve is already 19 degrees BEFORE they have hit their growth spurt, you can imagine how it can rapidly worsen once that growth spurt hits. Just as before when we calculated the chance of progression, as a child matures their risk of surgery decreases.
| Sanders Score | Curve Size | Curve Location | Probability of Surgery |
|---|---|---|---|
| 3 | 19 | Lumbar/thoracolumbar | 2.58% |
| 4+ | 19 | Lumbar/thoracolumbar | 0.34% |
| 3 | 19 | Any thoracic curve | 9.78% |
| 4+ | 19 | Any thoracic curve | 1.39% |
Looking for other warning signs
We know that major risk factors for a curve getting worse or needing surgery are:
- The size of the curve
- How skeletally mature the child is
- The location of the curve
However we also know that standard screening methods can be error prone, and it can be difficult to detect a mild scoliosis without using x-ray which has its own risks. Are there other warning signs or symptoms to keep an eye out for that would suggest a child has scoliosis?
Changes in Back Shape or Flexibility
We’ve talked before about the rib hump that is a hallmark feature of scoliosis and how it develops as a way to relieve tension on the tight spinal cord and nerves. As the body tries to provide the cord with the shortest path possible as the patient bends over (Adam’s forward bending test), the spine rotates resulting in the classic rib hump. However it is also possible that the back will simply be flat as the body tries to relieve tension and the patient won’t be able to bend over normally and touch the floor. Thus a noticeable lack of flexibility or a flat back when bending can be an early warning sign of scoliosis.
Another early warning sign can be found when looking at the hands and the feet. Having flat feet or being hyper-mobile is a sign that the ligaments are not as tight compared to your average individual. Ligament laxity (loose ligaments) or joint hyper-mobility can be an early warning sign of scoliosis because it means that the ligaments are more susceptible to any forces which might pull on them. In the case of idiopathic scoliosis where the nerves are tight, this increased nerve tension provides an extra “pulling” force that the ligaments may not be able to handle, resulting in a higher risk of scoliosis developing. In fact, in diseases like Marfan’s Syndrome 11 and Ehler’s Danlos Syndrome 12 where the soft connective tissues (ie. ligaments) are affected and loose we see scoliosis occurring quite often.
When should mild idiopathic scoliosis be treated?
If we know that even a mild scoliosis can get worse and sometimes need surgery, when is the best time to treat it? As we discussed earlier one of the biggest factors is how skeletally mature the child is. The less mature the child is when the curve is detected, the higher the risk and thus the more urgent it is to begin treating it to “stay ahead of the curve.” We know from current scientific research that when detection and intervention are done early, surgery can be prevented 13 and curves can be reduced long-term 15. However early treatment doesn’t always mean bracing as physiotherapeutic exercises (PSSE) can often help 14. Bracing can always be used later if necessary, and we know from science that bracing is effective at reducing curves and preventing surgery as well 2.
The biggest take home message here is simply that the earlier the scoliosis is caught and treated, the better the outcome. While using x-ray to monitor a mild scoliosis isn’t wise because of the radiation exposure, monitoring with alternative methods such as a weight bearing (standing) MRI can be easily done so that any changes to the curve are caught quickly. Treating early not only helps prevent any structural changes or contractures from forming, but also allows us to utilize that worrisome adolescent growth spurt to our advantage as a corrective force 3.
With early detection and early intervention idiopathic begins to look like any other treatable condition
Another important take home message that we can learn from our progression and surgical calculators is that treatment needs to be continued until skeletal maturity is reached. The more skeletally mature the child is, the lower the risk of progression and surgery. Thus if we treat a scoliosis and keep the curve small until the body has stopped growing, we can rest assured that our results will last a long time 15.
When we take the time to understand scoliosis; what can cause it; what influences it getting worse; when it tends to get rapidly worse; and when the risk for worsening is minimized; we can come up with a winning game plan for treatment. Combined with novel methods for early detection (ie. using standing MRI and looking for early warning signs), mild idiopathic scoliosis begins to look less like a boogeyman and more like any other treatable condition.
References
- Aulisa, A. G. et al. Effectiveness of school scoliosis screening and the importance of this method in measures to reduce morbidity in an Italian territory. Journal of pediatric orthopedics. Part B; 10.1097/BPB.0000000000000611 (2019).
- Weinstein, S. L., Dolan, L. A., Wright, J. G. & Dobbs, M. B. Effects of bracing in adolescents with idiopathic scoliosis. The New England journal of medicine 369, 1512–1521; 10.1056/NEJMoa1307337 (2013).
- Mehta, M. H. Growth as a corrective force in the early treatment of progressive infantile scoliosis. The Journal of bone and joint surgery. British volume 87, 1237–1247; 10.1302/0301-620X.87B9.16124 (2005).
- Chidambaran, V. et al. Predicting the pain continuum after adolescent idiopathic scoliosis surgery. A prospective cohort study. European journal of pain (London, England) 21, 1252–1265; 10.1002/ejp.1025 (2017).
- Halawi, M. J., Lark, R. K. & Fitch, R. D. Neuromuscular Scoliosis. Current Concepts. Orthopedics 38, e452-6; 10.3928/01477447-20150603-50 (2015).
- Karachalios, T. et al. Ten-year follow-up evaluation of a school screening program for scoliosis. Is the forward-bending test an accurate diagnostic criterion for the screening of scoliosis? Spine 24, 2318–2324 (1999).
- Simony, A., Hansen, E. J., Christensen, S. B., Carreon, L. Y. & Andersen, M. O. Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 25, 3366–3370; 10.1007/s00586-016-4747-2 (2016).
- Grossman, T. W., Mazur, J. M. & Cummings, R. J. An evaluation of the Adams forward bend test and the scoliometer in a scoliosis school screening setting. Journal of pediatric orthopedics 15, 535–538; 10.1097/01241398-199507000-00025 (1995).
- Lonstein, J. E. & Carlson, J. M. The prediction of curve progression in untreated idiopathic scoliosis during growth. The Journal of bone and joint surgery. American volume 66, 1061–1071 (1984).
- Dolan, L. A. et al. Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Development and Validation of a Prognostic Model in Untreated Adolescent Idiopathic Scoliosis Using the Simplified Skeletal Maturity System. Spine deformity 7, 890-898.e4; 10.1016/j.jspd.2019.01.011 (2019).
- Buchan, J. G. et al. Rare variants in FBN1 and FBN2 are associated with severe adolescent idiopathic scoliosis. Human molecular genetics 23, 5271–5282; 10.1093/hmg/ddu224 (2014).
- Shirley, E. D., Demaio, M. & Bodurtha, J. Ehlers-danlos syndrome in orthopaedics. Etiology, diagnosis, and treatment implications. Sports health 4, 394–403; 10.1177/1941738112452385 (2012).
- Fusco, C. et al. Low rate of surgery in juvenile idiopathic scoliosis treated with a complete and tailored conservative approach. End-growth results from a retrospective cohort. Scoliosis 9, 12; 10.1186/1748-7161-9-12 (2014).
- Berdishevsky, H. et al. Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Scoliosis and spinal disorders 11, 20; 10.1186/s13013-016-0076-9 (2016).
- Aulisa, A. G. et al. Curve progression after long-term brace treatment in adolescent idiopathic scoliosis. Comparative results between over and under 30 Cobb degrees – SOSORT 2017 award winner. Scoliosis and spinal disorders 12, 36; 10.1186/s13013-017-0142-y (2017).