Top Surgeons Reveal 5 Secret Insights for Avoiding Scoliosis Surgery
As parents and patients navigate the complex world of scoliosis treatment, it’s easy to feel overwhelmed by conflicting advice. But what if the key to avoiding surgery lies in the unspoken truths shared by leading surgeons? Drawing from real conversations with top experts, here are five “secrets” that highlight why non-surgical options deserve serious consideration—and how innovative approaches like the Silicon Valley Scoliosis Method can make a difference.
Secret Number 1: Contractures Must Be Addressed—But They Don’t Require Cutting
To straighten a spine during surgery, surgeons must first tackle contractures: the soft tissues around the spine that become rigid and inflexible after being held in a scoliotic position for extended periods. Ligaments, discs, muscles, and joint capsules gradually lose their normal shape and range of motion, creating strong resistance against returning to a straight alignment.
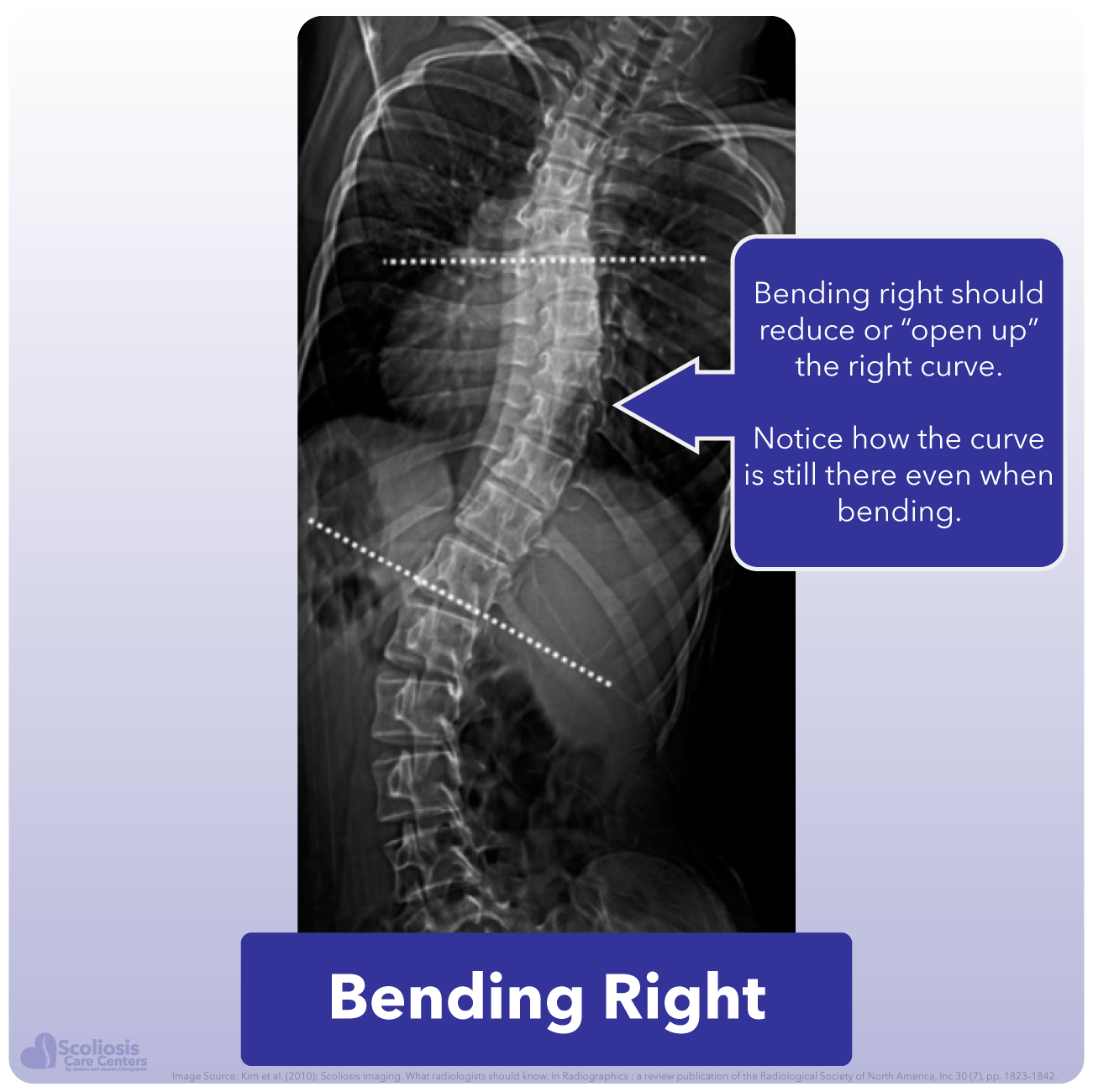
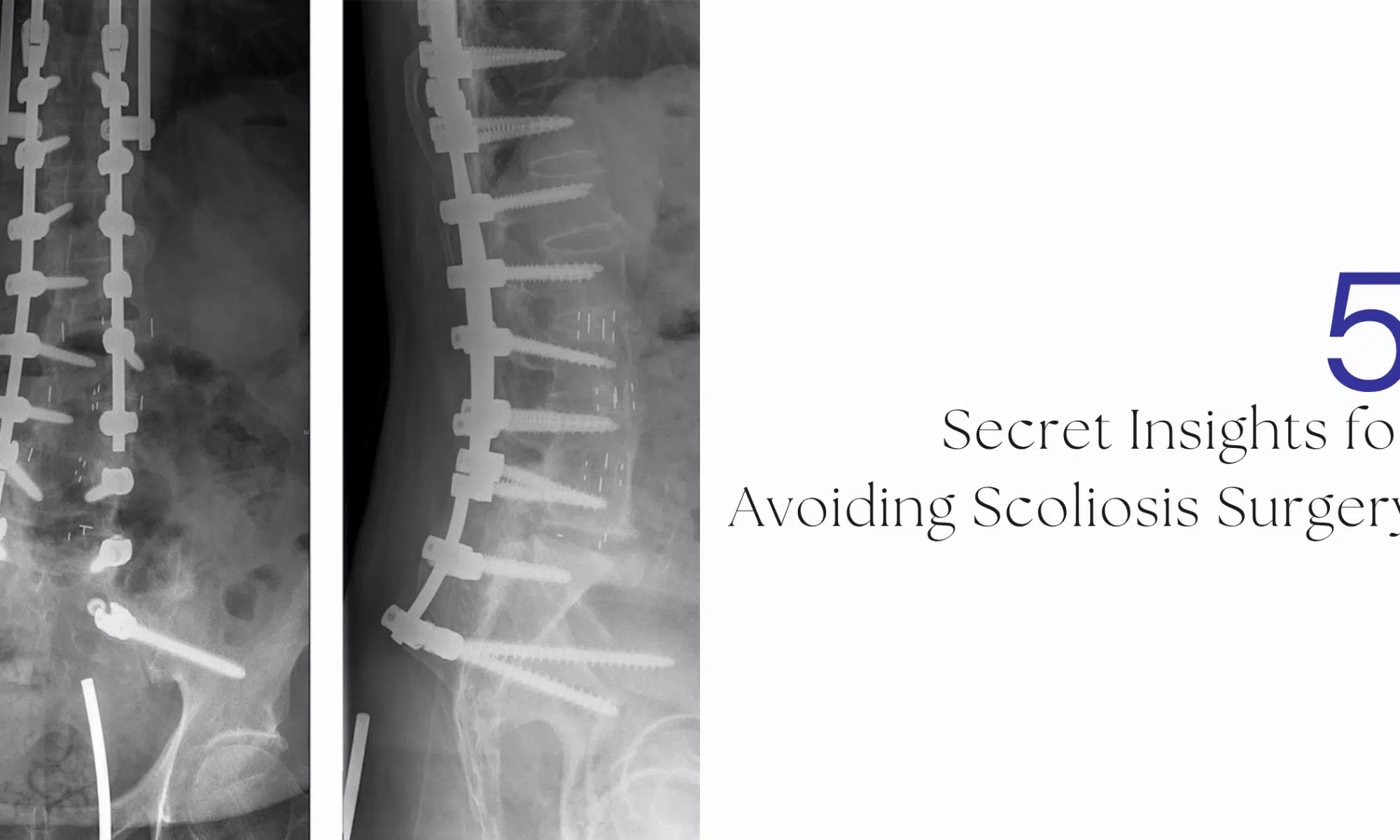
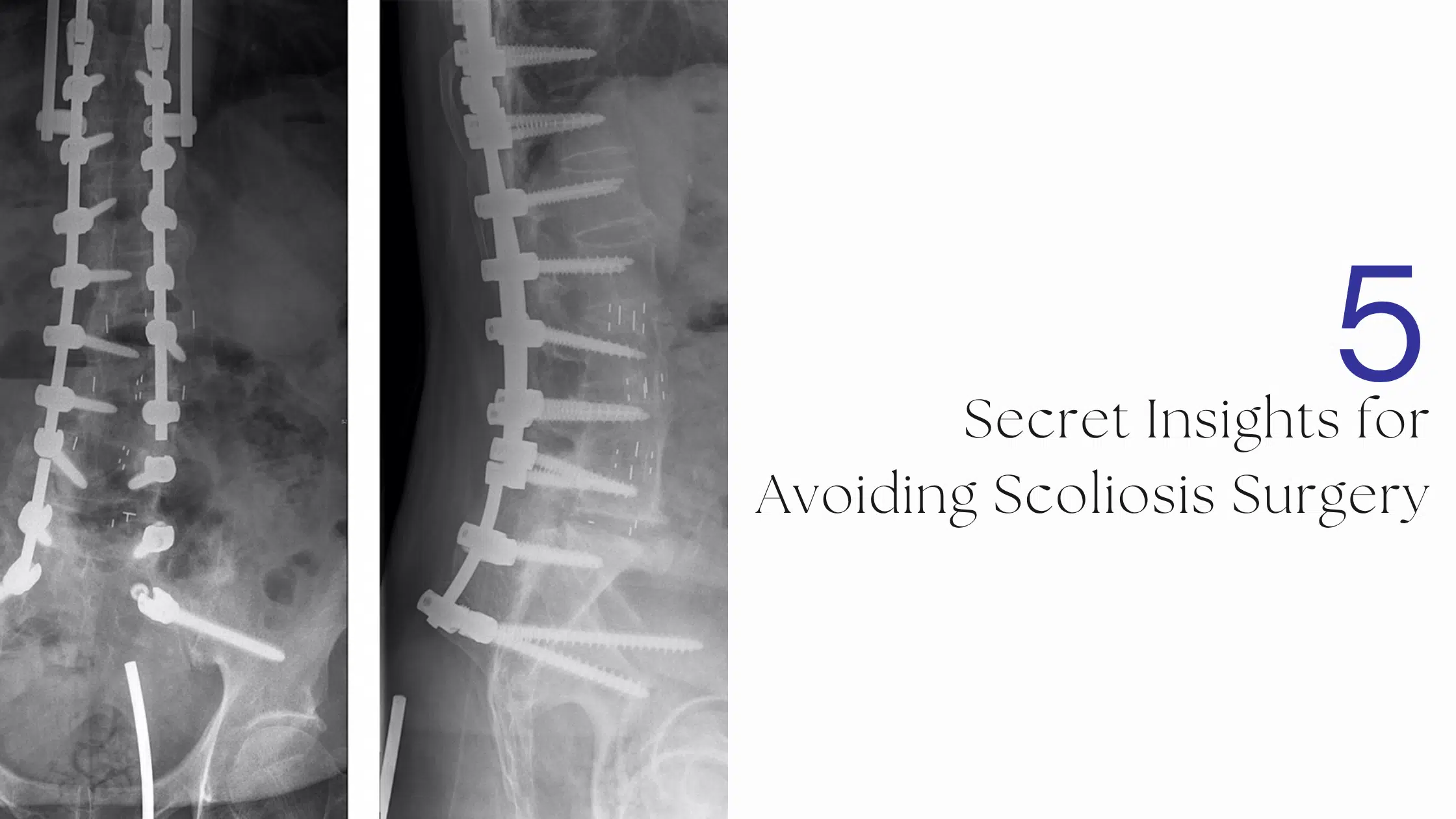
Here’s what a contractured spine looks like on an X-ray: Notice how, when the patient bends to the left, the spine remains stuck in a right-bent position? This immobility stems from contractures.
Surgeons address this by simply cutting them out—they sever ligaments, muscles, and joint capsules, even snapping off bone fragments or chiseling away facet joints. This destructive, irreversible process is euphemistically called “releasing contractures.” In reality, it permanently destroys parts of the spine that hinder straightening. Tragically, this aspect is often glossed over in patient discussions, hidden behind vague terms like “release.” It’s a shameful omission.
The good news? Contractures don’t need to be surgically excised. They can be stretched to restore normal flexibility. Silicon Valley doctors have invented the Scoliosis Flexibility Trainer, a non-surgical device that frees up the spine for better alignment. As part of the Silicon Valley Scoliosis Method, it offers a safer path to correction without the devastation of surgery.
Secret Number 2: The Short Spinal Cord Limits Straightening—And It May Be the Root Cause
Years ago, a mother brought her daughter—with an 80-degree scoliosis curve—to a top pediatric surgeon in Silicon Valley. The curve had started at 35 degrees, and despite trying every alternative treatment, it had progressed relentlessly. Devastated, the mom asked, “Can you still help? How straight can you make her spine now that it’s so severe?”
The surgeon’s reply was eye-opening: “I could make any spine perfectly straight, no matter how crooked, if it weren’t for the short spinal cord.”
As another expert elaborated, “Surgical correction is limited to spinal cord tolerance.” Even Dr. Harrington, inventor of the Harrington Rod, emphasized this principle. This is why spinal cord monitoring is standard in every scoliosis surgery—to ensure that straightening (which lengthens the spine) doesn’t overstretch the cord, risking ischemia or permanent damage.
This “short spinal cord” concept dates back to 1968, when the Roth hypothesis first proposed it as the primary explanation for idiopathic scoliosis. According to this theory, asynchronous growth—where the vertebral column elongates faster than the spinal cord—creates relative cord shortening. The resulting tension causes the spine to curve and rotate sideways, relieving strain by shortening the column’s effective length. Unlike tethered cord syndrome (a structural abnormality), this is a functional issue due to neuro-osseous mismatch, preceding scoliosis onset and driving progression.
All surgeons recognize this limitation, yet it’s rarely discussed openly. The key to avoiding surgery? Elongate the cord naturally and safely through targeted stretching techniques. This can prevent worsening and enable a straighter posture. Even if you’re skeptical about causation, the evidence is clear: The cord is short in scoliosis, it restricts straightening, and addressing it non-surgically could be transformative. What do you think?
Secret Number 3: The “Cascade of Surgeries” Is a Hidden Reality
Dr. Vericitas (name changed for anonymity), an adult neurosurgeon at a prestigious university hospital, once vented about the flaws in scoliosis care. In pediatric cases, the path often leads straight to fusion surgery, treated as the ultimate fix. Once fused, pediatric surgeons consider the job done—passing adult complications to specialists like him.
“And then begins the cascade of surgeries,” he lamented.
Stunned, I asked for clarification. “Yes, the surgery to fix the surgery to fix the surgery…” he confirmed, trailing off. In my 30 years in spine care, this was the first time a surgeon admitted it aloud. Eager to document it, I invited a colleague to witness, and Dr. Vericitas continued baring his soul about the system’s shortcomings.
“Would you go on record? Could we video this?” I asked.
His face paled in panic. “Oh no! I cannot go on the record with this!” The conversation ended abruptly.
I know what I heard: If he spoke publicly, he’d risk ostracism from colleagues and his employer. Thank you, Dr. Vericitas, for that rare moment of candor. It underscores a harsh truth—scoliosis surgery often isn’t a one-and-done solution but the start of ongoing interventions.
Secret Number 4: Surgery Can Worsen Pain Long-Term
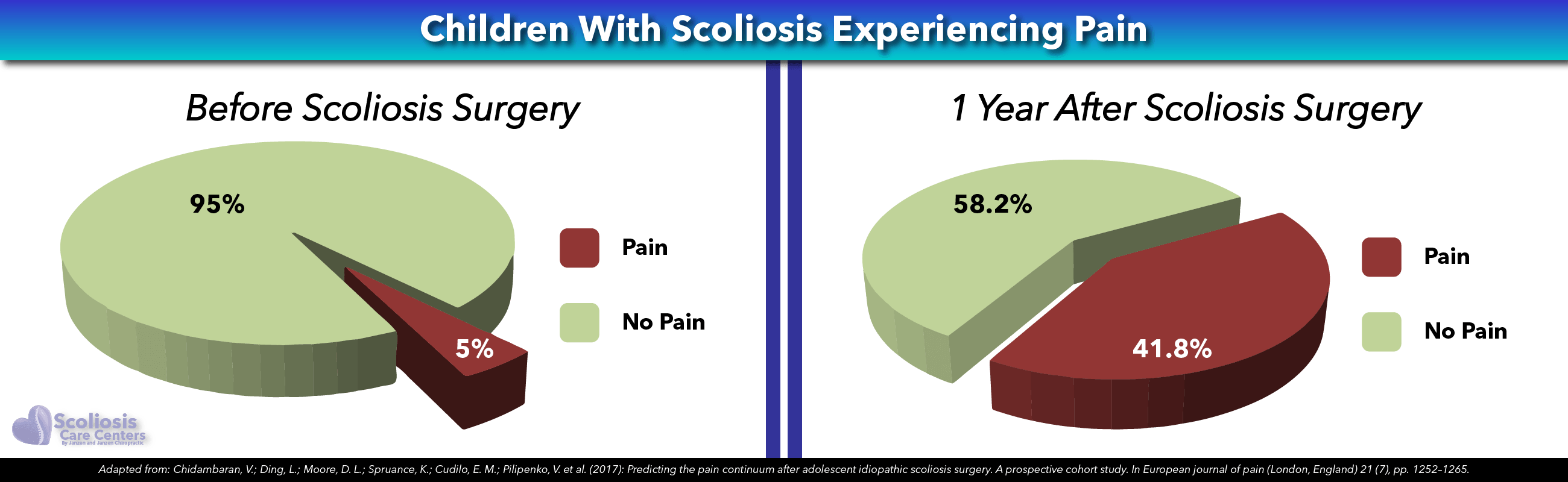
Contrary to the narrative that scoliosis surgery resolves issues within 3-6 months, evidence shows it can amplify pain. Researchers found that 42% of adolescents suffer debilitating pain one year post-surgery, compared to just 5% pre-surgery (Chidambaran et al., 2017). This study only counted pain rated 4/10 or higher, so the true incidence of chronic pain may be even greater.
Fusion alters spinal mechanics, potentially leading to adjacent segment degeneration, nerve irritation, or hardware issues—all contributing to persistent discomfort. This challenges the idea of surgery as a pain-reliever and highlights the need for non-invasive alternatives.
Secret Number 5: Many Surgeons Avoid Surgery for Their Own Kids
Given the choice, numerous surgeons opt for conservative, non-surgical treatments for their children’s scoliosis—avoiding surgery at all costs.
Recall Dr. Vericitas and his frustrations? He shared these insights while enrolling his own child in the Silicon Valley Scoliosis Method. When it’s their family, surgeons often prioritize less invasive options, knowing the risks of fusion firsthand. This insider preference speaks volumes: Non-surgical paths like bracing, exercises, and targeted therapies offer hope for better quality of life without lifelong complications.
Listening to What Surgeons Really Say
If we tune into the subtle messages from top scoliosis surgeons, a clear picture emerges: Soft-tissue contractures and the short spinal cord are major barriers to straightening—and must be addressed for success. (The Silicon Valley Scoliosis Method was built to tackle these directly.) Without targeting them, treatment plans often falter.
If it were their child, many surgeons would exhaust every non-surgical avenue to evade fusion’s destructive, irreversible effects—like cascades of revisions and increased pain. Instead, they’d seek innovative, conservative methods for a complication-free future.
Ultimately, these “secrets” teach us that avoiding surgery isn’t just possible—it’s often the wiser path, guided by the experts themselves.