Written and reviewed for scientific and factual accuracy by Dr. Austin Jelcick, PhD and Dr. Matthew Janzen, DC
It has long been believed that the earlier scoliosis can be caught, the better the possibility of preventing the need for invasive surgery. Recent research has indicated dramatic success with scoliosis curves when they are caught and treated before they reach 30 degrees. The success rate of our clinic is 100% for the curves under 30 degrees avoiding the need for surgery.
Failed Scoliosis Screening Efforts of the Past
The goal of scoliosis screening has traditionally been to attempt to catch the curves soon enough to prevent surgery. Considering how invasive surgery is, experts measure success in the number of adolescent scoliosis cases that can avoid surgery. The problem with current scoliosis screening methods is that they tend to catch the curves after they’ve already grown to a dangerously large size. Simply viewing a child’s back from behind while they bend can result in a high miss rate of small curves.
This forward bending test, also called the Adam’s Scoliosis Test, has been called by some the “Too Late” test.
When the state of California evaluated the effectiveness of school screening programs, no significant change in the rate scoliosis surgery could be observed.
Part of this ineffectiveness could be blamed on insensitive screening methods that catch problems too late, but the other part is rightfully blamed on a lack of effective non-surgical treatment. The most common strategy for orthopedic surgeons is to either “wait and see” if the curve grows worse a year later (it usually will), or to prescribe a Boston brace (notoriously ineffective braces). Based on this lack of effectiveness and a desire to save money, mandatory school screenings were canceled.
A New Method of Screening for Scoliosis
It is possible to detect the warning signs of looming scoliosis before the curve even begins. Paying attention to these warnings also aid in detecting small curves long before they become a big problem. We’ve designed our own screening protocol that goes far beyond the Adam’s forward bending test. Here are some of the screening practices that helping us catch even the smallest curves.

1. Screen for the Causes of Scoliosis
Scoliosis that occurs during growth can have 3 basic causes: Anatomic asymmetry1, neuromuscular disorders3, or tight nerves2. These root cause conditions can be screened for upon exam, and sometimes detected before a curve even begins. Screening for tight nerves is probably the most important early screen for scoliosis. One such test, which provides an easy way to tell if your child has tight nerves, is called the Cox Test. More information on how to screen for tight nerves using a Cox test can be found here.

2. Rate Ligament Laxity / Joint Hypermobility
When the nervous system is tight, it exerts a pulling force on the spine. A good way to measure how susceptible a patient is to the effects of nerve tension is to rate how flexible their ligaments are. Over-flexible, lax ligaments will be more susceptible to tight nerves and therefore more susceptible to the pull of those nerves causing scoliosis in the spine. This is why patients with conditions such as Marfan’s5 and Ehler’s Danlos Syndrome6 are at higher risk for scoliosis.One does not need to have a genetic condition to have hypermobile joints, as sometimes joint hypermobility occurs in absence of any known genetic disorder. We use the Beighton Hypermobility scale to assess a child’s ligament laxity, along with taking note of the presence of flat feet, or pes planus.
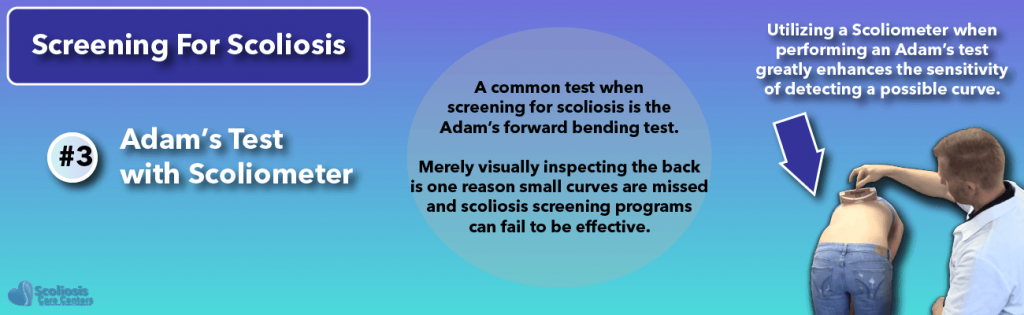
3. Adam’s Test with Scoliometer
In the past, it had been common practice to screen for scoliosis using the Adam’s forward bending test. The test was performed by depending only on the visual inspection of the back, and no special tools for measuring subtle asymmetries. Many small curves are missed this way, and this is in part why scoliosis screening programs lacked effectiveness. By utilizing a Scoliometer when performing Adam’s Forward Bending Test greatly enhances the sensitivity of detecting a possible curve.9
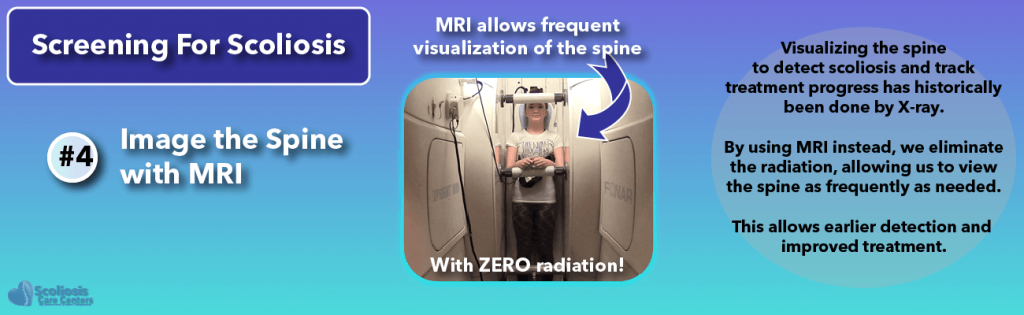
4. Use Standing MRI to Actually See What the Spine is Doing
If we really wanted to detect who has scoliosis with 100% accuracy, we would simply X-ray every kid’s spine several times a year.Why don’t we?Obviously, such frequent dosage of X-ray would be harmful. In the past, X-ray was the only way to truly see if a scoliosis was present. Thankfully today, a standing full spine MRI can be used instead of full spine X-ray. MRI is a 100% safe, radiation-free way to evaluate the spine. It can be performed as often as is desired to monitor the spine.
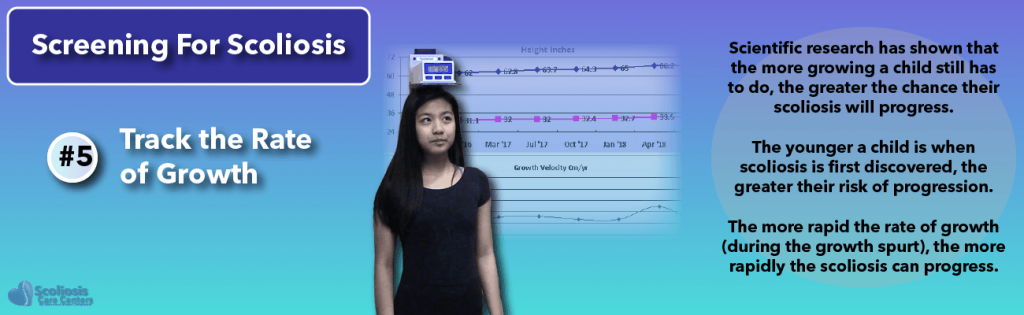
5. Track the Rate of Growth
We’ve said that scoliosis happens with growth. It is important to specify that the RATE of growth is the true factor. The faster the growth, the greater the risk. By tracking and graphing rate of growth, it alerts us to the periods of highest risk for scoliosis.
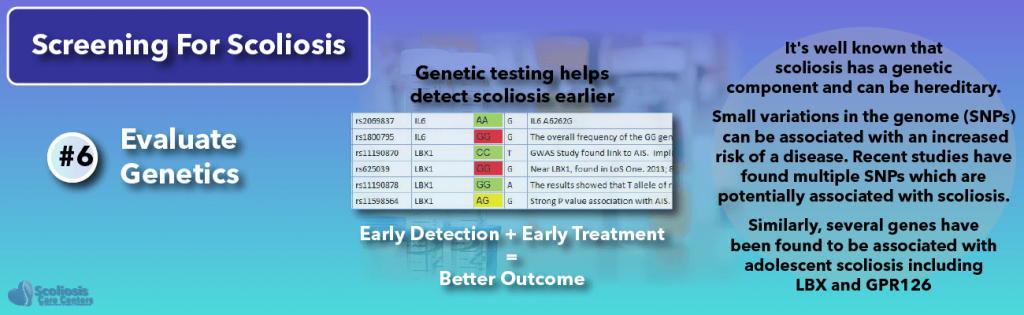
6. Evaluate the Genetics
It is well known that scoliosis has a genetic component and can be hereditary, or put another way, runs in the family. High-tech genetic tests are not even necessary to take advantage of this knowledge. If a family member has scoliosis, then it is a safe bet that there is an increased risk for the others. If someone has just a sibling or immediate family member with scoliosis, then there is a 19% chance that they will have it also4.
Studies have also helped pinpoint some of the genetic variances that are associated with adolescent idiopathic scoliosis. Much excitement surrounded the discovery that two particular genes, LBX7, and GPR1268, are both linked to adolescent scoliosis, and they both play key roles in the development and function of the nervous system. While whole-genome sequencing is coming down in price, many variances can be detected with a simple analysis of inexpensive DNA SNP tests.
Today, it is possible to cross-reference one’s ancestry DNA against known SNPs associated with adolescent scoliosis risk. Having the ability to understand and an individual’s genetic variances as they relate to scoliosis is becoming an increasingly powerful tool.
Closing comments regarding screening techniques
By utilizing the above screening method, our detection rate for every child screened is nearly perfect, as any doubt about the existence of a curve can be eliminated with radiation-free MRI of the spine. To date, cases that undergo the Silicon Valley Method treatment before their curves reach 30 degrees have a 100% success rate for avoiding surgical need. Early detection and early intervention with effective treatment truly may represent a preventive cure for scoliosis in growing spines.
References
- Kaspiris A, Grivas TB, Weiss H-R, Turnbull D. Surgical and conservative treatment of patients with congenital scoliosis, Α search for long-term results. Scoliosis 2011;6:12.
- Roth M. Idiopathic scoliosis from the point of view of the neuroradiologist. Neuroradiology 1981;21:133–8.
- Veldhuizen AG, Wever DJ, Webb PJ. The aetiology of idiopathic scoliosis, Biomechanical and neuromuscular factors. Eur Spine J 2000;9:178–84.
- Wise CA, Gao X, Shoemaker S, Gordon D, Herring JA. Understanding genetic factors in idiopathic scoliosis, a complex disease of childhood. Curr Genomics 2008;9:51–9.
- Buchan JG, Alvarado DM, Haller GE, et al. Rare variants in FBN1 and FBN2 are associated with severe adolescent idiopathic scoliosis. Hum Mol Genet 2014;23:5271–82.
- Shirley ED, Demaio M, Bodurtha J. Ehlers-danlos syndrome in orthopedics, Etiology, diagnosis, and treatment implications. Sports Health 2012;4:394–403.
- Li Y-L, Gao S-J, Xu H, et al. The association of rs11190870 near LBX1 with the susceptibility and severity of AIS, a meta-analysis. Int J Surg 2018.
- Liu G, Liu S, Lin M, et al. Genetic polymorphisms of GPR126 are functionally associated with PUMC classifications of adolescent idiopathic scoliosis in a Northern Han population. J Cell Mol Med 2018;22:1964–71.
- Cote P, Kreitz BG, Cassidy JD, Dzus AK, Martel J. A study of the diagnostic accuracy and reliability of the Scoliometer and Adam’s forward bend test. Spine (Phila Pa 1976) 1998;23:796-802; discussion 803.