Kyphosis and Hyperkyphosis
Written and reviewed for scientific and factual accuracy by Dr. Austin Jelcick, PhD and Dr. Matthew Janzen, DC. Last reviewed/edited on October 27, 2020. First published February 20, 2020.
If you open the dictionary, kyphosis is defined as the exaggerated outward curvature of the thoracic region of the spine which results in a rounded upper back. You may have also heard kyphosis, especially hyperkyphosis (more severe kyphosis) referred to as “hunchback.” While kyphosis and scoliosis can both occur, they are fundamentally two different problems. This article will discuss what it is, how common kyphosis occurs, where it typically occurs, why it happens and how it affects the body, as well as what can be done to treat it.
How common is kyphosis?
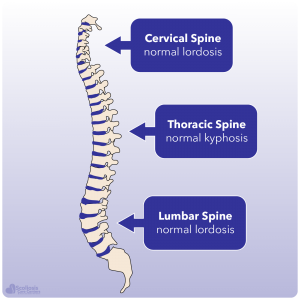
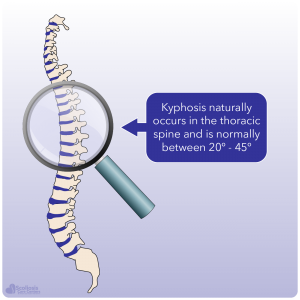
Unlike scoliosis where any significant (more than 10º) sideways (lateral) shift is thought to be problematic, kyphosis naturally occurs in the spine of healthy individuals. The key is THE SIZE of the kyphosis and determining whether or not the kyphosis falls into the normal range 1. When we look at a normal healthy spine, we can see that there is a natural kyphosis in the thoracic spine and a natural lordosis in the lumbar spine. For growing teens, a kyphosis of 20º – 40º is thought to be within the normal range; although this range is still currently debated 2,3.
Just as some degree of kyphosis is normal, it is also normal for kyphosis in the spine to gradually increase as we grow older. For example, 10 year old boys have an average of a 21º kyphosis while 10 year old girls have an average of 24º. As they grow, the kyphosis will increase to approximately 25º for boys and 26º for girls by age 19. By the time they have reached their 50’s, the average kyphosis is now 41º for men and 33º for women 4. In fact, this natural progression of kyphosis is well known is often referred to as age-related kyphosis.
Age-related kyphosis has an increased incidence the older we get. For every 10 years we age, the incidence of age-related kyphosis increases by about 6-11%. This age related progression is thought to be due to a combination of factors. These factors include a combination of poor posture, reduced strength of the back extensor muscles, and dehydration of the discs between each vertebrae 5.
Where does kyphosis occur?
In a normal spine, kyphosis will occur in the thoracic region. This is the natural location for it to occur because when we look at the upper (cervical) and lower (lumbar) regions of the spine we see a natural lordosis, or inward curvature in contrast to the kyphosis (outer curvature) in the thoracic region. These curves naturally balance each other and allow us to walk upright while our discs provide shock absorption as we walk, jog, and run. However we get into trouble when the kyphosis becomes larger than it should be or when it isn’t located in the thoracic area of the spine. Thus, any kyphosis in the thoracolumbar or lumbar region is considered to be abnormal 6.
Why does kyphosis happen?
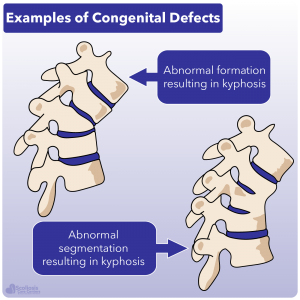
Before talk about how kyphosis occurs, it is important to know that there are DIFFERENT TYPES of kyphosis. Just how a scoliosis can be idiopathic, neuro-muscular, congenital, or syndromic, kyphosis can occur for different reasons. For example there can be congenital changes in the spine that occur during development that cause a vertebrae to be misshaped or where the vertebrae fail to properly segment normally, resulting in congenital kyphosis. There can be various neuro-muscular problems that can cause a kyphosis to occur, and even situations where a kyphosis arises due to a tumor or after an injury 7.
These congenital, neuro-muscular, and post-traumatic causes of kyphosis need to be distinguished from other types as they each have their own unique issues and contributing factors. For example, in athletic teens and those who do heavy lifting (ie. farm hands) kyphosis can occur but is known as “apprentice kyphosis.” This type is associated with repetitive activities involving carrying heavy weights (axial loading) when the spine is immature, but is not progressive and symptoms can usually resolve with time, rest, and changes to activities being performed 8,9.
In contrast, when a kyphosis that is larger than normal is present that doesn’t have one of these other causes, it is often referred to as hyperkyphosis or Scheuermann’s Hyperkyphosis when other diagnostic factors are found. Just as idiopathic scoliosis is commonly thought to have an unknown cause, Scheuermann’s hyperkyphosis has long been thought to have an unknown cause 10; however we will talk more about possible causes supported by research later on.
Scheuermann’s Hyperkyphosis
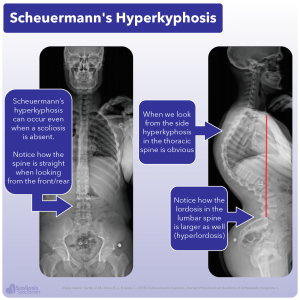
Scheuermann’s hyperkyphosis, sometimes simply called Scheuermann’s Disease, is diagnosed when the kyphosis is larger than 40º, is rigid, and when there are wedged vertebrae (wedge shaped) present. Specifically, for a diagnosis to be made there needs to be three or more adjacent vertebrae where anterior wedging is 5º or more 11,12. Just as with scoliosis, Scheuermann’s hyperkyphosis is thought to have some genetic component as it has been found to be hereditary, or able to be passed down from parent to child 11,12.
In the United States, Scheuermann’s occurs in about 1-8% of the population 12,13, and is typically diagnosed in kids 12-17 years old while rarely being seen in kids 10 years old or younger. The higher incidence in males versus females is also significant as it occurs approximately twice as often in males than females (in stark contrast to scoliosis which occurs more often in females) 11.
What causes Scheuermann’s Disease?
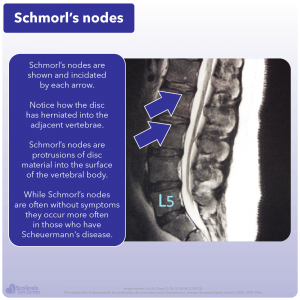
As we briefly mentioned before, it has long been thought that the cause of Scheuermann’s is unknown. However there have been numerous studies investigating its causes, and some more recent research that has shown promise in finally getting to the bottom of the problem. Over the years a wide range of hypotheses about the cause of Scheuermann’s have been studied ranging from death of bone tissue (osteonecrosis 14) and herniated discs (specifically Schmorl’s nodes 15) to osteoporosis 16; abnormal mechanical stresses causing changes in the bone (altered remodeling 17); and even altered composition of parts of the bones such as the endplates causing a disturbance in the normal vertical growth 2. Even being taller than average and increased levels of growth hormones 2,21 have been thought to contribute to the development of hyperkyphosis, yet each of these ideas have fallen short of providing a real cause.
As follow up studies have been performed, new research has debunked many of the potential causes of Scheuermann’s Hyperkyphosis. Death of bone tissue (osteonecrosis) for example has been found to be occurring in the wrong place for it to affect the development of kyphosis. Similarly, Schmorl’s nodes are seen in people without hyperkyphosis and there hasn’t been a significant difference found in the bone density of people with hyperkyphosis compared to those without it 15. Thus, as various ideas have arisen about what causes Scheuermann’s other studies have come out suggesting these ideas are incorrect or at the very least, incomplete.
While many potential causes have been rules out by research, studies still show that there is a genetic component 20 to the development of hyperkyphosis. Oddly enough, it has found that tight hamstrings appear to not only be related to hyperkyphosis, but are an important factor that directly influences the success of correcting it with surgery 19. It was thought that tight hamstrings can concentrate stress on the thoracic region of the spine 18,19, however there is likely more to it than just this. Keep this in mind for now as we will talk about this towards the end of the article and how this can suggest a common root cause with scoliosis as well.
How does hyperkyphosis affect the body?
Having a larger than normal curvature in the thoracic spine can affect the body in several ways. Before we talk about how Scheuermann’s Disease/hyperkyphosis can be symptomatic, the rigid nature of the kyphosis needs to be emphasized. As opposed to a kyphosis caused simply by bad posture which can be corrected, the hyperkyphosis associated with Scheuermann’s Disease will not resolve when lying on your back or on your stomach. Additionally, the lordosis in the lumbar region of the spine is typically increased, with the lordosis in the cervical region being increased sometimes as well 12,27.
As we briefly mentioned, patients with Scheuermann’s often have Schmorl nodes where the disc protrudes into the adjacent vertebrae, while the height of the discs are decreased 25. There are some changes when we look under the microscope at the bone such as abnormal vertebral endplate cartilage; irregular mineralization; and even increased ratios of proteoglycans to collagen. While all of this sounds extremely scientific, it can be simply summarized as this: there are changes in the structure/composition of the bone and cartilage associated with Scheuermann’s hyperkyphosis 26.
While changes to the bone and cartilage will occur, more noticeable symptoms will also occur with hyperkyphosis. Most teens will notice a cosmetic and/or postural deformity, especially when bending over. This “hump” when bending over is why hyperkyphosis is sometimes referred as “hunchback.” Accompanying this cosmetic issue can also be pain in the thoracic area (where the kyphosis is present) with no identifiable event causing the pain (example of an identifiable event: I lifted a heavy object and the next day my back hurt). This pain usually becomes worse during activity, and improves with rest 11. However it is important to note that people with Scheuermann’s hyperkyphosis have a two and half (2.5) times higher risk for having constant back pain compared to other people 28.
What happens when hyperkyphosis is left untreated?
When someone has Scheuermann’s doesn’t do anything to treat it, they do not have any major health problems when the kyphosis is less than 100º, while pulmonary function can be affected if the curve is larger than 100º. No significant difference has been found regarding missing work or school due to pain or other problems associated with the kyphosis, and no significant differences in daily activities, self-consciousness, self-esteem, or recreation activities have been found either 22. However people who have hyperkyphosis (average of 71º) tend to have more intense back pain, less range of motion of trunk extension (see image for example), and tend to have jobs that require less activity 22.
Will a kyphosis get worse?
We talked earlier about how as we age, our natural kyphosis tends to increase in size but can be influenced by things such as bad posture and weakening of the back muscles. While kyphosis tends to progress with age, the chances that the hyperkyphosis associated with Scheuermann’s gets worse has been unknown for decades16. While only a few long term studies have looked at if and when Scheuermann’s will progress, based on the limited data it would seem that it doesn’t progress more than what we would expect from the natural age related progression.
If you remember from our discussion on age-related kyphosis, we talked about how a boy with a 21º kyphosis at age 10 will likely have a 41º kyphosis by the time he is 50 years old; while a girl with a 24º at age 10 would have a 33º kyphosis by age 50. So essentially, we can expect a kyphosis to naturally increase by about 10-20º over a period of 40 years. When we look at people with Scheuermann’s hyperkyphosis we see about the same: an average curve size of 46º increased to 60º over an average of 46 years while the wedging of the vertebrae increased from 8.8º to 9.9.º 29. What is also interesting is that despite the progression of the curve there was no difference in function (muscle strength, balance, and coordination), and progression did not predict any symptoms.
Can kyphosis be cured?
By now it should be clear that there is a natural and normal amount of kyphosis that occurs in the spine which is important for our body to perform daily activities like walking and running. It should also be fairly obvious that in most cases, even a large curve like what occurs with Scheuermann’s hyperkyphosis doesn’t cause a lot of problems other than pain. So if reversing a kyphosis is bad because we need some amount of naturally occurring kyphosis, and most cases are not severe enough to warrant surgery, what can be done to treat it?
You will be pleased to hear that research has shown hyperkyphosis can be effectively and successfully reduced and treated by with conservative approaches 27. This includes specific physio-therapeutic exercises and can also include bracing to help reduce the curve. Similar to scoliosis however, hyperkyphosis is best treated with conservative approaches when the patient is young and skeletally immature. For example, when it is treated before skeletal maturity, and average kyphosis of approximately 63º can be reduced to about 36.5º through bracing 30.
As far as exercises are concerned, those that strengthen the back, and in particular Schroth exercises have been shown to prevent progression and reduce the size of the curve 31. Using corrective exercises such as these appear to promote stability, and a more upright posture as well, helping to prevent future progression caused by bad posture 32. The biggest take home message regarding the treatment of hyperkyphosis is that SURGERY IS RARELY NEEDED, with the majority of patients seeing success with conservative treatment 10.
Indications for treatment
We know from the research that conservative treatments including bracing and physiotherapeutic exercises are successful in treating and managing Scheuermann’s hyperkyphosis, but WHEN should it be treated? Many people will seek treatment once the kyphosis progresses, when pain occurs, or when the cosmetic appearance becomes undesirable. Because neurologic and cardiopulmonary complications rarely occur with hyperkyphosis, its is very rare for treatment to be sought for these reasons 15.
Typical treatments aside from bracing and physiotherapeutic exercises include anti-inflammatory medication as well as postural improvement exercises. Postural improvement exercises and trunk extensor strengthening may not reduce the size of the kyphosis, but can help reduce pain and improve physical conditioning 1,33. Similar to scoliosis treatment is most effective when the spine is still growing before it has reached maturity. Considering that hyperkyphosis is associated with scoliosis 12,27 beginning treatment while a child/teen is still skeletally immature is a wise idea.
Hyperkyphosis and scoliosis: A common root cause?
We’ve talked about how research has shown scoliosis to be associated with hyperkyphosis, and also how research has shown people with hyperkyphosis to have tight hamstrings. But what could tight hamstrings suggest? More importantly, how do tight hamstrings link scoliosis and hyperkyphosis?
Numerous scientific studies have shown that “tight hamstrings” are not only associated with hyperkyphosis 2,22-24, but are an important factor that surgeons need to consider when they perform a surgical correction of a hyperkyphosis 19. If a surgeon neglects this key factor, they can over-correct the curve and cause even more imbalance 19. While earlier studies thought that tight hamstrings cause the thoracic spine to encounter more stress leading to the development of a hyperkyphosis, the problem may not be with the hamstrings at all but the nerves instead.
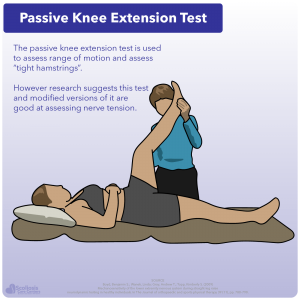
To understand how tight nerves could be mistaken as tight hamstrings, we need to first see how you would determine if hamstrings were tight in the first place. Doctors and clinicians will perform passive knee flexion, something commonly known as a passive knee extension test. This test will determine the range of motion of the knee, and also is used to test for tight hamstrings. However, recent research suggests this test actually is good at assessing tight nerves 34.
The body has natural ways to protect itself when it is exposed to stresses. Think of how when you injure your leg or foot how you will naturally limp in an effort to protect the injury. Mechanosensitivity is thought to be one of the normal protective responses of nerves (peripheral nerves) to mechanical stresses they encounter during movement. The more sensitive the nerves are to the limbs (arms, legs) moving, the higher the mechanosensitivity. A common test for this in the lower quarter of the body is the straight leg raise (SLR test) just as was done to test “tight hamstrings.”
What is being affected: muscle, nerve or both?
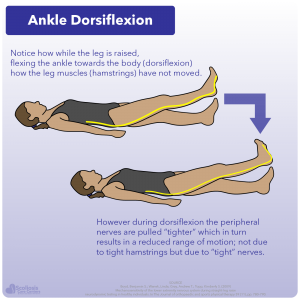
The key to determining that the peripheral nerves are sensitive or tight is that when the straight leg raise is performed by a clinician is in the angle of the ankle during the leg raise. When the ankle is flexed towards the body (dorsiflexion) during the straight leg raise, it results in more tightness and tension 34 and the amount the leg could raise is decreased; but why? How would simply flexing the ankle cause the stretch to feel stronger and reduce range of motion?
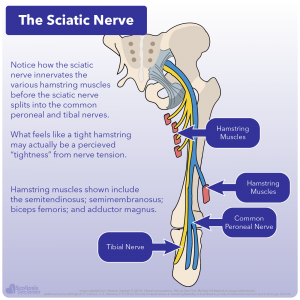
The answer is NOT tight hamstrings, but instead is related to the nervous system and tight nerves and/or short spinal cord. If we look at the anatomy of the body and specifically at the hamstrings and where the nerves are located, we see that the hamstring muscles are innervated by the sciatic nerve (part of the peripheral nerves) before it subsequently splits off into the tibal and common peoneal nerve. If someone is stretching (such as the straight leg raise) and they feel a tightness or burning in their hamstrings, this could be due to tight hamstrings but it could also be THE NERVES that are causing this sensation as they too are stretched.
Think about what is happening when the individual flexes their ankle/foot during the straight leg raise. The leg and the hamstrings have not moved: only the foot and ankle have moved during dorsiflexion. Yet when dorsiflexion is performed, more of a stretch; tightness; tension; and burning are felt and the amount the leg can be raised decreases 34. This strongly suggests that the cause of the increased “stretch” and the decreased range of motion is due to the nerves and nerve tension.
While it has long been thought that the range of motion of a joint is limited by muscle tension (tightness), this does not appear to be true where non-muscular tissues (such as nerves) are stretched as well. Given the hamstrings are innervated by the non-muscular tissue that is the sciatic nerve, it is reasonable to think that if this nerve was tight, stiff or otherwise limited in it ability to stretch that we would see a reduced range of motion. Similarly it would make sense that if we stretch the nerves we could increase range of motion.
This is exactly what we see happen as when the sciatic nerve is stretched, the muscles (hamstring and others) are not affected, yet we see that the range of motion during dorsiflexion is increased 35. Given that “tight hamstrings” are an important factor to consider when straightening a kyphosis surgically, it would seem that the issue is NOT tight hamstrings but is ACTUALLY nerve tension in disguise. This is profound given that in scoliosis surgical correction of a curve is limited by the short/tight spinal cord and suggests that kyphosis and scoliosis share a common underlying problem: nerve tension. This also provides insight as to why hyperkyphosis may occur with scoliosis given the shared problem of short/tight nerves.
Who To See and What To Do About Kyphosis
We’ve talked a lot about kyphosis and hyperkyphosis: what it is, how it happens, how it affects the body, and more. Kyphosis is a natural curve in the spine but can become more severe than it should be, becoming hyperkyphosis which has its own problems. As we discussed previously it is rare for hyperkyphosis to need intervention aside from the desire to change cosmetic appearances. However we also talked about how hyperkyphosis and scoliosis share the common problem of nerve tension which can be misinterpreted as muscle tension (tight hamstrings).
Nerve tension, such as that due to a short spinal cord an be a significant problem and a driving force for scoliosis, as well as hyperkyphosis. While hyperkyphosis may only warrant treatment to correct appearance, the underlying issue of nerve tension should be paid close attention to as it can result in more severe problems such as the development of a large scoliosis curve. Especially in young, skeletally immature children and teens, nerve tension poses a problem that can quickly worsen during periods of rapid growth (growth spurts). Thus, monitoring and addressing the problem of nerve tension through safe, targeted stretching (neuro-elongation) is a good proactive/preventative action to take.
This isn’t to say that a hyperkyphosis or scoliosis will be completely prevented, but the driving force of nerve tension would be reduced, slowing any progression which may occur. Combined with frequent monitoring (ie. standing, weight bearing MRI), this proactive approach is a great start in preventing hyperkyphosis, scoliosis, and their associated issues from “sneaking up” and allows for early intervention and non-surgical treatment to maximize results and success.
References
- Wenger, D. R. & Frick, S. L. Scheuermann kyphosis. Spine 24, 2630–2639; 10.1097/00007632-199912150-00010 (1999).
- Lowe, T. G. Scheuermann disease. The Journal of bone and joint surgery. American volume 72, 940–945 (1990).
- Tribus, C. B. Scheuermann’s kyphosis in adolescents and adults. Diagnosis and management. The Journal of the American Academy of Orthopaedic Surgeons 6, 36–43; 10.5435/00124635-199801000-00004 (1998).
- Fon, G. T., Pitt, M. J. & Thies, A. C. Thoracic kyphosis. Range in normal subjects. AJR. American journal of roentgenology 134, 979–983; 10.2214/ajr.134.5.979 (1980).
- Jang, H.-J., Kim, M.-J. & Kim, S.-Y. Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis. Journal of physical therapy science 27, 1161–1164; 10.1589/jpts.27.1161 (2015).
- Bradford, D. S. Moe’s textbook of scoliosis and other spinal deformities. 2nd ed. (W.B. Saunders, Philadelphia, London, 1987).
- Yaman, O. & Dalbayrak, S. Kyphosis and review of the literature. Turkish Neurosurgery 24, 455–465; 10.5137/1019-5149.JTN.8940-13.0 (2014).
- Greene, T. L., Hensinger, R. N. & Hunter, L. Y. Back pain and vertebral changes simulating Scheuermann’s disease. Journal of pediatric orthopedics 5, 1–7; 10.1097/01241398-198501000-00001 (1985).
- Blumenthal, S. L., Roach, J. & Herring, J. A. Lumbar Scheuermann’s. A clinical series and classification. Spine 12, 929–932 (1987).
- Weiss, H.-R., Turnbull, D. & Bohr, S. Brace treatment for patients with Scheuermann’s disease – a review of the literature and first experiences with a new brace design. Scoliosis 4, 22; 10.1186/1748-7161-4-22 (2009).
- Mansfield, J. T. & Bennett, M. StatPearls. Scheuermann Disease (Treasure Island (FL), 2020).
- Makurthou, A. A. et al. Scheuermann disease. Evaluation of radiological criteria and population prevalence. Spine 38, 1690–1694; 10.1097/BRS.0b013e31829ee8b7 (2013).
- Palazzo, C., Sailhan, F. & Revel, M. Scheuermann’s disease. An update. Joint, bone, spine : revue du rhumatisme 81, 209–214; 10.1016/j.jbspin.2013.11.012 (2014).
- BICK, E. M. & COPEL, J. W. The ring apophysis of the human vertebra; contribution to human osteogeny. II. The Journal of bone and joint surgery. American volume 33-A, 783–787 (1951).
- Wood, K. B., Melikian, R. & Villamil, F. Adult Scheuermann kyphosis. Evaluation, management, and new developments. The Journal of the American Academy of Orthopaedic Surgeons 20, 113–121; 10.5435/JAAOS-20-02-113 (2012).
- Bradford, D. S., Brown, D. M., Moe, J. H., Winter, R. B. & Jowsey, J. Scheuermann’s kyphosis. A form of osteoporosis? Clinical Orthopaedics and Related Research, 10–15 (1976).
- Weinstein, S. L. The Pediatric spine. Principles and practice / editor, Stuart L. Weinstein. Vols 1-2 (Raven Press, New York, 1994).
- Lambrinudi, C. ADOLESCENT AND SENILE KYPHOSIS. British medical journal 2, 800-820.2; 10.1136/bmj.2.3852.800 (1934).
- Hosman, A. J. et al. Scheuermann kyphosis. The importance of tight hamstrings in the surgical correction. Spine 28, 2252–2259; 10.1097/01.BRS.0000085097.63326.95 (2003).
- Halal, F., Gledhill, R. B. & Fraser, C. Dominant inheritance of Scheuermann’s juvenile kyphosis. American journal of diseases of children (1960) 132, 1105–1107; 10.1001/archpedi.1978.02120360061011 (1978).
- Skogland, L. B., Steen, H. & Trygstad, O. Spinal deformities in tall girls. Acta orthopaedica Scandinavica 56, 155–157; 10.3109/17453678508994344 (1985).
- Bradford, D. S., Moe, J. H. & Winter, R. B. Kyphosis and postural roundback deformity in children and adolescents. Minnesota medicine 56, 114–120 (1973).
- Fisk, J. W. & Baigent, M. L. Hamstring tightness and Scheuermann’s disease a pilot study. American journal of physical medicine 60, 122–125 (1981).
- Murray, P. M., Weinstein, S. L. & Spratt, K. F. The natural history and long-term follow-up of Scheuermann kyphosis. The Journal of bone and joint surgery. American volume 75, 236–248; 10.2106/00004623-199302000-00011 (1993).
- Aufdermaur, M. Juvenile kyphosis (Scheuermann’s disease). Radiography, histology, and pathogenesis. Clinical Orthopaedics and Related Research, 166–174 (1981).
- Zaidman, A. M. et al. The mode of inheritance of Scheuermann’s disease. BioMed research international 2013, 973716; 10.1155/2013/973716 (2013).
- Tomé-Bermejo, F. & Tsirikos, A. I. Conceptos actuales sobre la enfermedad de Scheuermann. Presentación clínica, diagnóstico y controversias sobre su tratamiento. Revista espanola de cirugia ortopedica y traumatologia 56, 491–505; 10.1016/j.recot.2012.07.002 (2012).
- Ristolainen, L. et al. Untreated Scheuermann’s disease. A 37-year follow-up study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 21, 819–824; 10.1007/s00586-011-2075-0 (2012).
- Ristolainen, L., Kettunen, J. A., Kujala, U. M., Heinonen, A. & Schlenzka, D. Progression of untreated mild thoracic Scheuermann’s kyphosis – Radiographic and functional assessment after mean follow-up of 46 years. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association 22, 652–657; 10.1016/j.jos.2017.03.009 (2017).
- Etemadifar, M. R., Jamalaldini, M. H. & Layeghi, R. Successful brace treatment of Scheuermann’s kyphosis with different angles. Journal of Craniovertebral Junction & Spine 8, 136–143; 10.4103/jcvjs.JCVJS_38_16 (2017).
- Bezalel, T., Carmeli, E., Levi, D. & Kalichman, L. The Effect of Schroth Therapy on Thoracic Kyphotic Curve and Quality of Life in Scheuermann’s Patients. A Randomized Controlled Trial. Asian spine journal 13, 490–499; 10.31616/asj.2018.0097 (2019).
- Senthil, P., Sudhakar, S., Radhakrishnan, R. & Jeyakumar, S. Efficacy of corrective exercise strategy in subjects with hyperkyphosis. Journal of back and musculoskeletal rehabilitation 30, 1285–1289; 10.3233/BMR-169668 (2017).
- Zaina, F. et al. Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth. Hyperkyphosis, junctional kyphosis, and Scheuermann disease. European journal of physical and rehabilitation medicine 45, 595–603 (2009).
- Boyd, B. S., Wanek, L., Gray, A. T. & Topp, K. S. Mechanosensitivity of the lower extremity nervous system during straight-leg raise neurodynamic testing in healthy individuals. The Journal of orthopaedic and sports physical therapy 39, 780–790; 10.2519/jospt.2009.3002 (2009).
- Andrade, R. J. et al. The potential role of sciatic nerve stiffness in the limitation of maximal ankle range of motion. Scientific reports 8, 14532; 10.1038/s41598-018-32873-6 (2018).