Scoliosis Risk Calculator
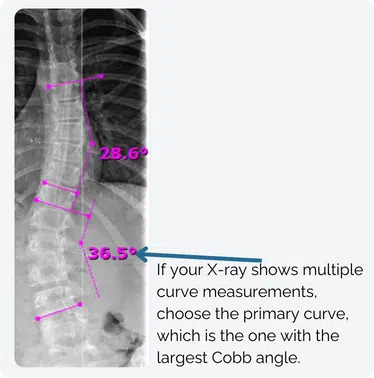
What is a Cobb Angle?
The Cobb angle measures the severity of a scoliosis curve, based on an X-ray or MRI taken from the back (posteroanterior view). To measure it, doctors identify the most tilted vertebrae above and below the curve’s apex and draw perpendicular lines. The angle formed is the Cobb angle. Larger Cobb angles are linked to higher risks of scoliosis progression and surgery.
Ready to Take Action?
After calculating your risk, consult with a case diresctor for a no charge case review.
No Charge Case ReviewLearn More About Scoliosis Treatment
Medical Disclaimer
The Scoliosis Risk Calculator is a tool designed to provide general information and estimates regarding scoliosis progression and potential surgical risks based on the input provided. It is not intended to diagnose scoliosis, predict individual outcomes, or replace professional medical advice, diagnosis, or treatment.
Use of this tool implies your acknowledgment of these limitations and acceptance of the information provided as general guidance only.
Scientific References
- Bunnell, W. P. (1986): The natural history of idiopathic scoliosis before skeletal maturity. In Spine 11 (8), pp. 773–776.
- Charles, Yann Philippe; Daures, Jean-Pierre; Rosa, Vincenzo de; Diméglio, Alain (2006): Progression risk of idiopathic juvenile scoliosis during pubertal growth. In Spine 31 (17), pp. 1933–1942. DOI: 10.1097/01.brs.0000229230.68870.97.
- Cheung, Jason Pui Yin; Cheung, Prudence Wing Hang; Samartzis, Dino; Luk, Keith Dip-Kei (2018): Curve Progression in Adolescent Idiopathic Scoliosis Does Not Match Skeletal Growth. In Clinical Orthopaedics and Related Research 476 (2), pp. 429–436. DOI: 10.1007/s11999.0000000000000027.
- Cousminer, Diana L.; Berry, Diane J.; Timpson, Nicholas J.; Ang, Wei; Thiering, Elisabeth; Byrne, Enda M. et al. (2013): Genome-wide association and longitudinal analyses reveal genetic loci linking pubertal height growth, pubertal timing and childhood adiposity. In Human molecular genetics 22 (13), pp. 2735–2747. DOI: 10.1093/hmg/ddt104.
- Dimeglio, Alain; Canavese, Federico (2013): Progression or not progression? How to deal with adolescent idiopathic scoliosis during puberty. In Journal of children’s orthopaedics 7 (1), pp. 43–49. DOI: 10.1007/s11832-012-0463-6.
- Dolan, Lori A.; Weinstein, Stuart L.; Abel, Mark F.; Bosch, Patrick P.; Dobbs, Matthew B.; Farber, Tyler O. et al. (2019): Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Development and Validation of a Prognostic Model in Untreated Adolescent Idiopathic Scoliosis Using the Simplified Skeletal Maturity System. In Spine deformity 7 (6), 890-898.e4.
- Lipman, Terri H.; Cousounis, Pamela; Grundmeier, Robert W.; Massey, James; Cucchiara, Andrew J.; Stallings, Virginia A.; Grimberg, Adda (2016): Electronic Health Record Mid-Parental Height Auto-Calculator for Growth Assessment in Primary Care. In The Journal of Clin Pediatr (Phila) (Clinical Pediatrics), 55(12), 1100–1106. 10.1177/0009922815614352
- Lonstein, J. E.; Carlson, J. M. (1984): The prediction of curve progression in untreated idiopathic scoliosis during growth. In The Journal of bone and joint surgery. American volume 66 (7), pp. 1061–1071.
- Melmed, Shlomo; Polonsky, Kenneth S.; Larsen, P. Reed; Kronenberg, Henry (2016): Williams textbook of endocrinology. Philadelphia, PA: Elsevier.
- Sanders, James O.; Khoury, Joseph G.; Kishan, Shyam; Browne, Richard H.; Mooney, James F.; Arnold, Kali D. et al. (2008): Predicting scoliosis progression from skeletal maturity. A simplified classification during adolescence. In The Journal of bone and joint surgery. American volume 90 (3), pp. 540–553.
- Tan, Ken-Jin; Moe, Maung Maung; Vaithinathan, Rose; Wong, Hee-Kit (2009): Curve progression in idiopathic scoliosis. Follow-up study to skeletal maturity. In Spine 34 (7), pp. 697–700. DOI: 10.1097/BRS.0b013e31819c9431.