Written and reviewed for scientific and factual accuracy by Dr. Austin Jelcick, PhD and Dr. Matthew Janzen, DC
Scientific studies have shown idiopathic scoliosis to have a higher potential for worsening based on the amount of growing a child has left to do; that is, the growth potential of the child4. Another way of thinking about this is that scoliosis has a higher risk of progression in skeletally immature children.
What does skeletally immature mean?
As a child grows and matures, their spine along with the rest of their skeleton grows and matures as well. Let’s pause here and quickly differentiate between bone growth and bone maturity.
Growth, in terms of bone, refers to the changes in size and mass (ie. the length of a bone, width, its weight, etc.) over time3 which can be quantified. Maturity on the other hand (bone maturity) refers to the changes a bone undergoes as its structure/organization changes; including structural changes (the shape of the bone) as well as mineralization of the bone such as at its ends (the epiphyses)12. It is this difference in definitions that allows two children to have the same bone age without the same chronological age (ie. 7 years old) as children develop at different rates. Similar to this, bone age is not associated with a particular stage of puberty (or when puberty will begin) similar to that of chronological age10. Despite this, bone age is still utilized in predicting the onset of puberty.
How is bone age and skeletal maturity measured?
Skeletal maturity is commonly measured utilizing one of several methods including the Greulich-Pyle method; the Tanner-Whitehouse method; the Thumb Ossification Composite Index (TOCI); the Sanders scale; and the Risser sign (which may also be called Risser stage). Each method differs, however the overall concept remains the same: An x-ray is taken and based on the x-ray, an evaluation of skeletal age is performed.
While the Greulich-Pyle and Tanner-Whitehouse methods evaluate bone age based on x-rays of the wrist and hand, the Risser sign evaluates bone age based on the degree of fusion and ossification (the process of laying down new bone) of the pelvic bones (which include the iliac bones)9. Many scientific studies have been performed to assess the reliability and accuracy of each method with the take home message remaining the same: No method is perfect in predicting bone age or likelihood of scoliosis progression, but all are useful in estimating bone/skeletal age7, 8, 13, 14.
However, progression of scoliosis occurs during growth when the skeleton is immature and continues until skeletal maturity, with intervention during early skeletal age being preferable6, 2. It should also be noted that progression after skeletal maturity occurs has been observed in untreated individuals1, 15
How do I assess or understand a Risser sign?
Evaluating Risser sign to help estimate bone age (and thus skeletal maturity and risk for scoliosis progression) is easily done during a spine x-ray as the pelvis is imaged at the time of the spine. If you remember from the previous section, the iliac bones make up a portion of the bones of the pelvis and are the bones assessed when determining Risser sign. Specifically, the Risser sign evaluates the new bone ossifying along the ilium on a scale of 1 to 5 as visualized below:

A Risser scale of 0 corresponds to an immature skeleton of someone with a lot of growing left to do, and no ossification is observed along the ilium. As they go through puberty, new bone is laid down until they reach Risser 5, at which point all new bone has fused to the ilium and now appears as one solid bone.
How are the Risser scale and risk for scoliosis progression related?
As we have discussed previously, the younger and more skeletally immature the child, the greater the risk for progression; that is, the lower the Risser (ie. Risser 0) at the time a scoliosis curve is observed; the greater the risk the scoliosis will progress. As the final stage of puberty has been observed to occur on or after Risser 2 11, let’s look at this further breaking down risk by Risser scale:
RISSER 0: Young skeletal age; up to the onset of puberty; at beginning of the adolescent growth spurt
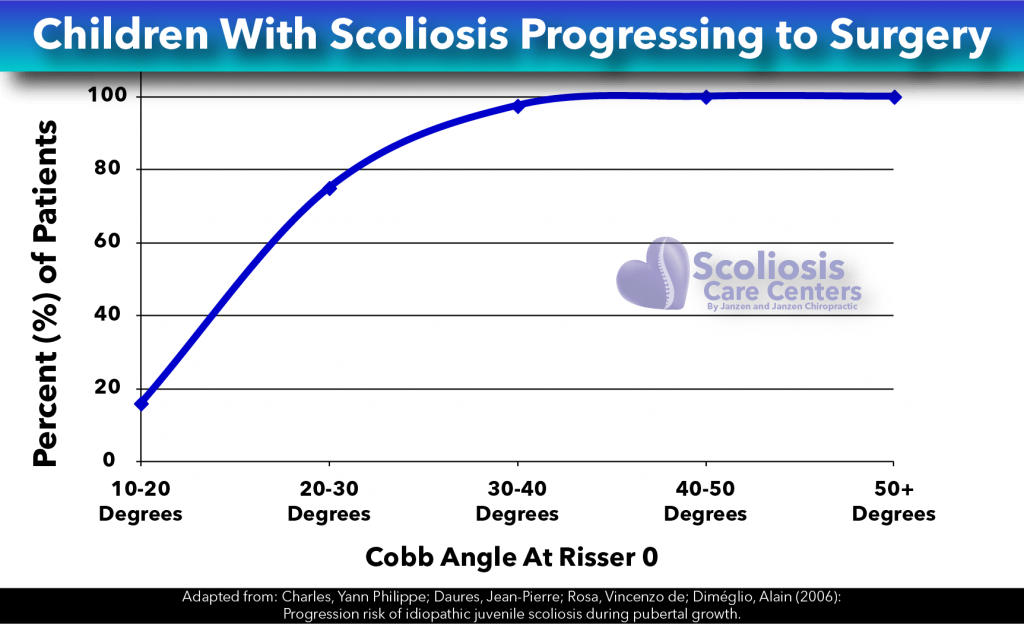
A scientific study published in Spine5 observed over two hundred children with scoliosis and followed the progression of their scoliosis. For those with curves less than 20 degrees at the start of puberty, only 16% required surgery. For children with curves 20-30 degrees at the start of puberty, THE NUMBERS DRASTICALLY CHANGE. An astounding 75% of these patients now required surgery. Similarly, for children with curves greater than 30 degrees at the start of puberty, 100% of children with curves greater than 30 degrees at the beginning of puberty requiring surgery.
RISSER 0-2: Up to the mid-point of the adolescent growth spurt
If a child’s curve is over 25 degrees, and has a Risser score of 0-2 (skeletally immature), they have a 58% chance of progressing beyond 50 degrees according to the BRAIST study by Weinstein et al. performed in 2013. To help illustrate this, observe this risk for progression in the following chart adapted from the study by Nachemson et al. describing the progression rate for children ten to sixteen years old with curves of various sizes (see table):
| Curve Magnitude | Age and Associated Progression Rate | ||
|---|---|---|---|
| 10-12 Years | 13-15 Years | 16 Years | |
| < 19º | 25% | 10% | 0% |
| 20º – 29º | 60% | 40% | 10% |
| 30º – 39º | 90% | 70% | 30% |
| 60º | 100% | 90% | 70% |
You can see in the table above that BOTH the size of the scoliosis curve as well as the age of the patient were directly related to the rate of progression: the younger the patient and the larger the curve, the more likely the scoliosis would progress. Nachemson et al. also found that bracing was 40% more effective than observation only in preventing progression of more than 6 degrees; despite the poorly fit braces of the time (1995).
RISSER 3-4: The rate of rapid progression begins to drop off for kids that are in the Risser 3-4 groups.
Looking at the table below taken from a study by Lonstein et al. we again see that as the child progresses towards adulthood and skeletal maturity, the less likely their scoliosis is to progress. We also again see that progression is also linked to the size of the initial curve as well as the age of the patient.
| Percentage Chance of Scoliosis Progression Based on Curve Size and Age at First Exam | ||
|---|---|---|
| Age First Examined | 5º – 19º Cobb Angle | 20º – 29º Cobb Angle |
| 10 and younger | 45% | 100% |
| 11-12 | 23% | 61% |
| 13-14 | 8% | 37% |
| 15 and older | 4% | 16% |
Take Home Messages
Estimating the skeletal maturity in children and teens with scoliosis is crucial in determining their likelihood of progression. Scientific studies have shown time and time again that the risk of scoliosis progression drastically increases based on the size of the curve as well as the degree of skeletal maturity of the patient. Because children grow and mature at different rates, two 11 year olds can have drastically different skeletal/bone ages and thus different risks of progression.
The Risser sign/scale can be utilized as a gauge of how mature a child’s skeleton is similar to other methods of estimating bone/skeletal age. We can utilize Risser to estimate how much growing they still have to do; how much their scoliosis may worsen if no action is taken; and also how much of the pubertal growth spurt is left to utilize as a corrective force.
References
- Ascani, E.; Bartolozzi, P.; Logroscino, C. A.; Marchetti, P. G.; Ponte, A.; Savini, R. et al. (1986): Natural history of untreated idiopathic scoliosis after skeletal maturity. In Spine 11 (8), pp. 784–789.
- Aulisa, Angelo G.; Guzzanti, Vincenzo; Falciglia, Francesco; Giordano, Marco; Galli, Marco; Aulisa, Lorenzo (2018): Brace treatment of idiopathic scoliosis is effective for a curve over 40 degrees, but is the evaluation of Cobb angle the only parameter for the indication of treatment? In European journal of physical and rehabilitation medicine. DOI: 10.23736/S1973-9087.18.04782-2.
- Baroncelli, Giampiero I.; Bertelloni, Silvano (2010): The Effects of Sex Steroids on Bone Growth. In Eric S. Orwoll, John P. Bilezikian, Dirk Vanderschueren (Eds.): Osteoporosis in men. The effects of gender on skeletal health / [edited by] Eric S. Orwoll, John P. Bilezikian, Dirk Vanderschueren. 2nd ed. Amsterdam, Boston: Elsevier/Academic Press, pp. 105–118.
- Bunnell, W. P. (1986): The natural history of idiopathic scoliosis before skeletal maturity. In Spine 11 (8), pp. 773–776.
- Charles, Yann Philippe; Daures, Jean-Pierre; Rosa, Vincenzo de; Diméglio, Alain (2006): Progression risk of idiopathic juvenile scoliosis during pubertal growth. In Spine 31 (17), pp. 1933–1942. DOI: 10.1097/01.brs.0000229230.68870.97.
- Cheung, Jason Pui Yin; Cheung, Prudence Wing Hang; Samartzis, Dino; Luk, Keith Dip-Kei (2018): Curve Progression in Adolescent Idiopathic Scoliosis Does Not Match Skeletal Growth. In Clinical Orthopaedics and Related Research 476 (2), pp. 429–436. DOI: 10.1007/s11999.0000000000000027.
- Hung, Alec Lik-Hang; Shi, Benlong; Chow, Simon Kwoon-Ho; Chau, Wai-Wang; Hung, Vivian Wing-Yin; Wong, Ronald Man-Yeung et al. (2018): Validation Study of the Thumb Ossification Composite Index (TOCI) in Idiopathic Scoliosis. A Stage-to-Stage Correlation with Classic Tanner-Whitehouse and Sanders Simplified Skeletal Maturity Systems. In The Journal of bone and joint surgery. American volume 100 (13), p. 88. DOI: 10.2106/JBJS.17.01271.
- Liu, D.; Xia, S. Q.; Shi, B.; Shi, B. L.; Liu, Z.; Sun, X. et al. (2018): Reliability and repeatability analysis of simplified skeletal maturity scoring and thumb ossification composite index in the assessment of skeletal maturity inadolescent idiopathic scoliosis. In Zhonghua yi xue za zhi 98 (43), pp. 3479–3484. DOI: 10.3760/cma.j.issn.0376-2491.2018.43.004.
- Manzoor Mughal, Arsalan; Hassan, Nuzhat; Ahmed, Anwar (2014): Bone age assessment methods. A critical review. In Pakistan journal of medical sciences 30 (1), pp. 211–215. DOI: 10.12669/pjms.301.4295.
- Melmed, Shlomo; Polonsky, Kenneth S.; Larsen, P. Reed; Kronenberg, Henry (2016): Williams textbook of endocrinology. Philadelphia, PA: Elsevier.
- Negrini, Stefano; Donzelli, Sabrina; Aulisa, Angelo Gabriele; Czaprowski, Dariusz; Schreiber, Sanja; Mauroy, Jean Claude de et al. (2018): 2016 SOSORT guidelines. Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. In Scoliosis and spinal disorders 13, p. 3. DOI: 10.1186/s13013-017-0145-8.
- Orwoll, Eric S.; Bilezikian, John P.; Vanderschueren, Dirk (Eds.) (2010): Osteoporosis in men. The effects of gender on skeletal health / [edited by] Eric S. Orwoll, John P. Bilezikian, Dirk Vanderschueren. 2nd ed. Amsterdam, Boston: Elsevier/Academic Press.
- Sanders, James O.; Khoury, Joseph G.; Kishan, Shyam; Browne, Richard H.; Mooney, James F.; Arnold, Kali D. et al. (2008): Predicting scoliosis progression from skeletal maturity. A simplified classification during adolescence. In The Journal of bone and joint surgery. American volume 90 (3), pp. 540–553. DOI: 10.2106/JBJS.G.00004.
- Sitoula, Prakash; Verma, Kushagra; Holmes, Laurens; Gabos, Peter G.; Sanders, James O.; Yorgova, Petya et al. (2015): Prediction of Curve Progression in Idiopathic Scoliosis. Validation of the Sanders Skeletal Maturity Staging System. In Spine 40 (13), pp. 1006–1013. DOI: 10.1097/BRS.0000000000000952.
- Weinstein, S. L.; Ponseti, I. V. (1983): Curve progression in idiopathic scoliosis. In The Journal of bone and joint surgery. American volume 65 (4), pp. 447–455.

